Ever wonder why elderly people tend to fall more? How can a person's mobility impact their quality of life? As physical therapists, these are questions we try to answer for our patients every day. As we age, our gait changes and affects our balance, safety, and overall function. Of course, our gait eventually affects our quality of life and can inhibit the joys that should be associated with the so-called “golden years.” Truthfully, anyone who is 70 and over that is experiencing any mobility issues should seek further education and even a formal gait analysis to determine an action plan to maintain their goals.
What is a gait analysis?
The official definition of gait analysis is, “the systematic study of human locomotion, usually by trained physical therapists, using instruments to measure body movements, body mechanics, and the activity of the muscles.” A classic representation of the gait cycle is much like the illustration below.
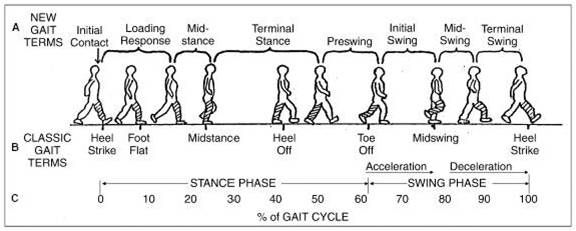
Detailed analysis of each gait phase can be found and described here.
The gait cycle is complex and confusing even to the well-trained clinician. There is no shame in not fully understanding or memorizing every minuscule detail. In fact, understanding and correcting every gait dysfunction may not have the impact on the patient that you expect. The second half of the equation is understanding the clinical significance of a particular disfunction and ultimately how it affects safety. As you might expect, not all gait dysfunctions or metrics have the same clinical impact. So, what are the critical data points from the gait cycle that provide the greatest impact on our patients’ lives?
Gait Speed
There are two major data points that are easily obtained. The first is gait speed or gait velocity, which is often referred to as the sixth vital sign. Research has shown that gait speed can help predict overall functional independence and can aid decision-making during a patient’s discharge.Gait speed can effectively predict assistive device needs, dependence levels for Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs), and of course, current and future fall risk. As demonstrated by the chart below, gait speed is directly correlated with patient independence.
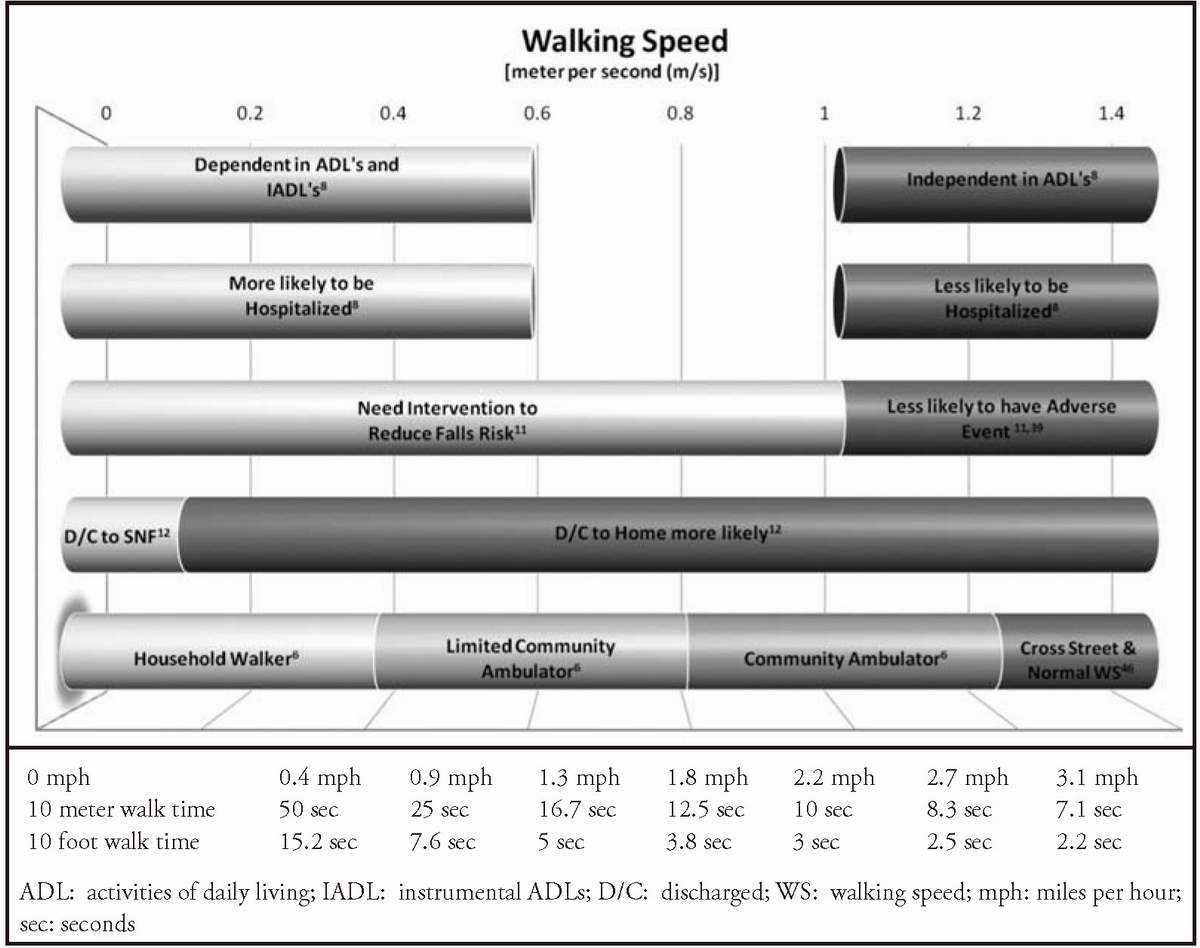
Maintaining current gait speeds, or improving speed, can have a significant impact on our patients’ fall risk, safety, and independence. In fact, CMS has indicated that just .08 meters per second (m/s) change in gait speed is clinically significant regarding fall risk. Specifically, every .1 m/s gained in speed can lower the fall risk by 7%. This indicates even the smallest of changes in speed can have a positive or negative impact on a person's fall risk and life.
Using gait speed to determine functional decline has hard data to back it up. Patients who walk slower than 0.6 m/s have an elevated risk of physical disability which can lead to a decline in health and function. Multiple studies have indicated that lower gait speed can correlate to higher mortality rates over 2- and 5-year periods within the aging population. For example, men aged 85 years who walk 0.85 m/s have a five-year survival rate of 85% while their same-age counterparts who walk 0.4 m/s have only a 40% chance of living five more years. With these statistics, it is easy to see why gait speed is considered the sixth vital sign. The good news is minor changes can have a significant impact on our patients' lives.
Cadence
Cadence is the second major data point that should be examined, as it directly correlates to gait speed and has a substantial impact on fall risk. Cadence is the number of steps a patient can take per minute. Typically, an increase in cadence is associated with lower fall risks.
Most often, if a person falls while walking, they fall forward. When an individual has a higher step cadence, it provides more opportunity for the person to take a “recovery step” forward if they begin to fall.
Conversely, long strides typically decrease cadence and increase fall risk due to larger step length and less limb speed to take that “recovery step”. Your patient can increase overall gait speeds with longer strides, but they may be putting themselves more at risk. Therefore, correlating gait speed and cadence is important for the clinician to fully understand in what way the patient is more at risk for falls.
Using AI for accurate Gait Analysis
By utilizing technologies like VSTBalance, clinicians can identify mobility deficits in older adults to determine if they are at risk of falling within the next 12 months. It uses artificial intelligence and machine vision to collect hundreds of data points including gait speed and cadence to help clinicians determine the best course of treatment to improve overall function and stay healthy. Regular assessments with VSTBalance ensure that patient progression can be tracked with confidence.


